How Long Does It Take for Your Throat to Heal after a Choke Stroke Treatment?
When someone has a stroke, one area many don’t think about right away is the throat. If you or a loved one has had a stroke and now have difficulty swallowing, hoarseness or a “tight feeling” in the throat, you’re not alone—and you probably have a lot of questions. How long will it take to heal? Will you ever be able to swallow normally again? And what role does a specialist in Choke Stroke Treatment Honolulu play in that healing journey?
In this article we’ll walk through the timeline for throat (or more precisely, swallowing-throat) recovery after a stroke, what factors affect it, and what you can do to help the process along. We’ll use simple language, analogies, and personal touch so even if you’re not medically trained you’ll feel empowered in your recovery.
1. Understanding what “throat healing” means after a stroke
When we talk about a “throat healing” after a stroke, we’re really talking about swallowing function and throat-muscle coordination rather than simply a sore throat. The medical term you’ll often see is Dysphagia—difficulty swallowing.
Think of it like a bridge: the mouth sends food and drink across the “bridge” of the throat to the esophagus and then the stomach. A stroke may damage the “support pillars” (the nerves and muscles) causing the bridge to wobble or even collapse. The “healing” means rebuilding that bridge so food and liquid move safely and smoothly again.
This kind of recovery isn’t always straightforward—it depends a lot on how the stroke affected the swallowing muscles, how quickly therapy starts, and how consistent the support and exercises are.
2. Why swallowing and throat function go off track after a stroke
Here are the key reasons:
- The brain controls swallowing through many signals. A stroke can interrupt those signals — especially if it hits the brainstem, motor cortex, or nerves linked to the throat muscles.
- The muscles of the throat (pharynx), mouth, voice box (larynx) might weaken or get uncoordinated.
- You may lose the protective reflexes—so when you swallow, food or liquid might go into the airway (a dangerous event called aspiration).
- Because of swallowing trouble, you might eat less, feel tired, and avoid food—this slows recovery.
So this isn’t just a “scratchy throat” like when you catch a cold—it’s a functional challenge that can impact nutrition, safety and quality of life.
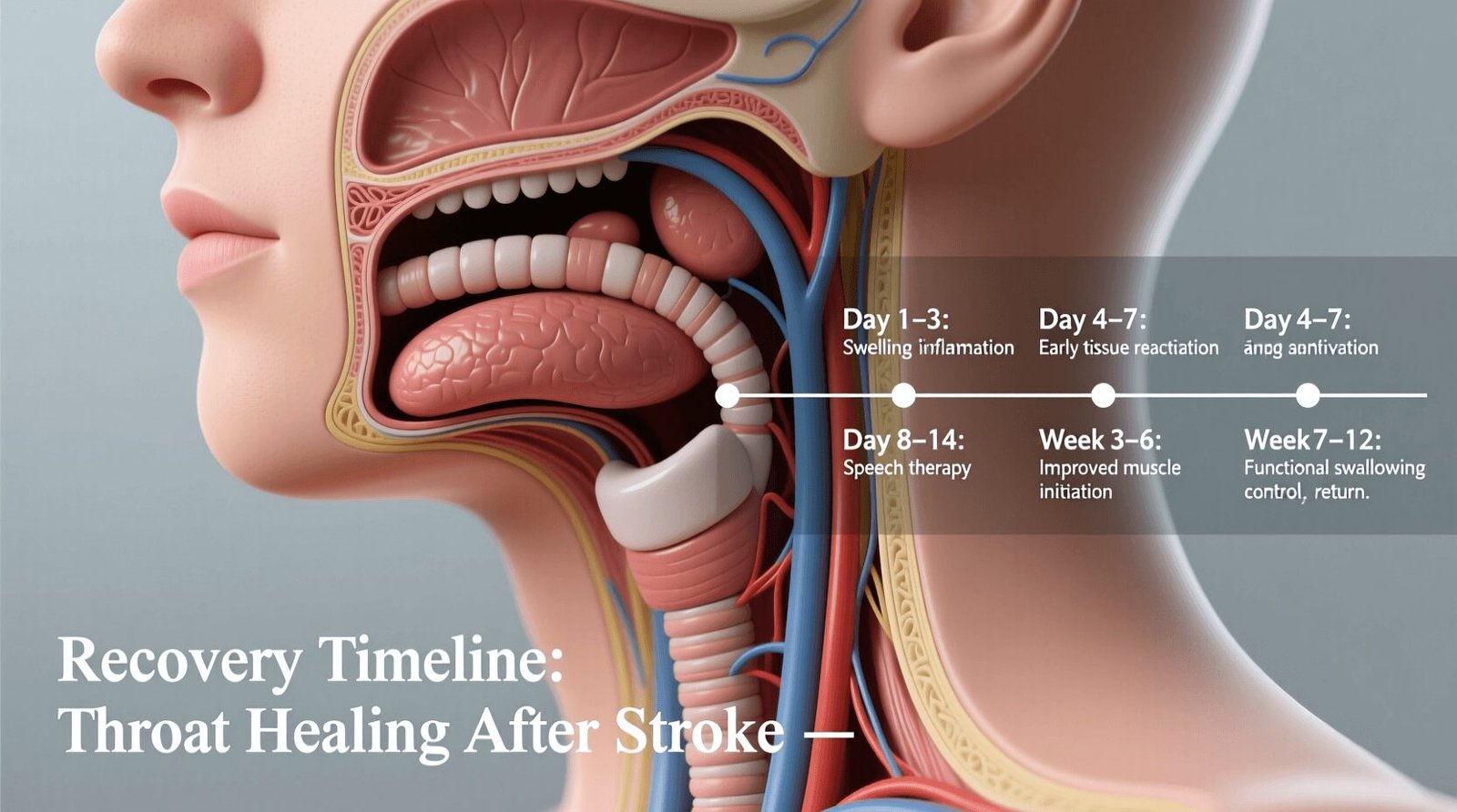
3. Typical time-frames: What the research says
So: how long does it take for the throat-swallowing function to heal after a stroke? The honest answer: it varies a lot. But research gives us some ballpark figures.
- Some studies indicate that over half of acute stroke patients with dysphagia recover within the first two weeks.
- Good news: the vast majority regain safe swallowing within weeks to months. For example: “most stroke patients can recover within a matter of weeks or months.”
- A guideline review found that swallowing therapy conducted for at least six months shows meaningful benefit and recommended therapy at least 3 times per week.
In everyday terms:
- In mild cases, you might see noticeable improvement in 1-4 weeks, especially with therapy.
- In moderate cases, improvement may stretch to 3-6 months.
- In more severe cases (large stroke, brainstem involvement), it can take 6-12 months or more, and full pre-stroke function may not always return—but very good function often is possible.
It’s like planting a garden: some plants sprout quickly in days, others take months to fully bloom. The “throat garden” needs the right soil (therapy), watering (exercise) and time.
4. Factors that speed up or slow down recovery
What makes a difference in how quickly you heal? Key ones:
Speed-up factors:
- Early intervention: The sooner you start swallowing therapy (within days to a week) the better.
- Mild initial impairment: If the dysphagia is mild, recovery tends to be faster.
- Good general health and nutrition: A body well-fed and rested heals faster.
- Good support at home: Family encouragement, safe eating practices, consistent exercises.
Slow-down factors:
- Severe stroke or involvement of brainstem or large areas controlling swallowing.
- Delay in therapy or inadequate therapy (low frequency).
- Other complications like pneumonia, aspiration, malnutrition.
- Poor posture, poor diet, low motivation or cognitive issues complicating therapy.
So think of recovery like hiking a mountain: the trail is easier with good gear, fresh food and a guide. It’s harder if you set off late, tired, with bad equipment.
5. The role of therapy and the specialist in Choke Stroke Treatment Honolulu
Here’s where the phrase Choke Stroke Treatment Honolulu becomes relevant. “Choke” is an informal way to capture risk of choking or aspiration after stroke—so if you live in Honolulu or nearby, you’d be looking for specialists and centres that treat swallowing problems after stroke.
What therapies are key?
- A speech-language pathologist (SLP) will assess your swallowing, posture, safe food textures, and teach exercises.
- Specific swallowing exercises: e.g., chin-tuck, effortful swallow, vocal cord adduction.
- Postural strategies and food/liquid texture modifications to reduce the risk of choking or aspiration.
- Advanced treatments: e.g., pharyngeal electrical stimulation (PES) has shown promise in severe dysphagia after stroke.
If you’re in Honolulu (or any location) the key is to seek a team that understands post-stroke swallowing problems (not just general throat pain). The team may include a neurologist, SLP, dietician and possibly otolaryngologist.
6. Practical steps you can take at home
Recovery is a team effort—and you are on the team. Here are things you can do:
- Sit upright when you eat or drink. Prevents “wrong turn” into airway.
- Take small bites, chew thoroughly, sip slowly.
- Use thickened liquids or soft foods if recommended (temporarily) so the “bridge” is less shaky.
- Practice dedicated swallowing exercises every day, as instructed by your therapist.
- Stay well-hydrated and well-nourished—muscles need fuel to repair.
- Monitor for signs of trouble (coughing, gurgly voice, food stuck) and report them.
- Keep a log of progress: which foods you try, how it feels, any improvement. This helps your therapists fine-tune treatment.
Treat it like physical rehab for a limb—you’re re-training muscles and nerves in your throat. Repetition matters.
7. Eating, drinking and diet adjustments during recovery
Your diet becomes part of your healing process. Some specifics:
- Start with softer foods (mashed potatoes, applesauce) and gradually move towards normal textures when safe.
- Thicken liquids if saliva or thin liquids go down wrong path.
- Avoid very hard, crunchy foods until you’re more secure with swallowing.
- Maintain good oral hygiene—poor mouth care increases pneumonia risk.
- Use mealtime as social time—positive context helps motivation.
Think of it like learning to walk again—but for your mouth and throat: you may start with training wheels (soft food, thick liquids), then go to unassisted walking (normal diet) when safe.
8. Mental and emotional impacts of throat/swallowing issues
It’s not just a physical challenge—having trouble swallowing after a stroke can affect your confidence, social life and mental health.
- You may feel anxious about choking in public.
- You might avoid eating with friends because you feel self-conscious.
- Fatigue and slower meals can affect your mood.
- Celebrate small milestones: a full meal, drinking without coughing, trying a new food.
Your support network (family, friends, rehab team) plays a big role. Recovery is holistic: body + mind.
9. Questions to ask your therapist or doctor
- “How severe is my swallowing difficulty and what’s the realistic timeline for improvement?”
- “What specific swallowing exercises should I be doing every day?”
- “Do I need diet modifications now — soft foods, thickened liquids?”
- “How often will I be re‐assessed for swallowing function?”
- “Is there advanced therapy available here or how do I access a specialist in Choke Stroke Treatment Honolulu (or in my area)?”
- “What warning signs should I look for that my throat or swallowing situation is worsening?”
- “When can I progress to more challenging foods or liquids safely?”
Conclusion
Recovering your throat and swallowing function after a stroke might feel like a slow climb, but with the right team, tools and mindset, you can make meaningful progress. It’s a blend of physical rehab, safe eating habits, patience and emotional resilience. If you’re based in Honolulu (or anywhere else), seeking specialised care in Choke Stroke Treatment Honolulu is a smart step to ensure you’re not just managing symptoms but truly rebuilding your swallowing “bridge”. Keep going—one bite, one sip, one swallow at a time.
FAQs
Q1: How soon after a stroke should swallowing therapy begin?
Therapy should start as early as possible—ideally within the first week if swallowing issues are identified—because early rehab tends to improve outcomes.
Q2: Can my throat recovery be complete or will I always have some limitation?
Many people regain safe swallowing and return to a normal diet, but recovery depends on stroke severity and individual factors. Some residual limitations may persist, but they can often be managed well.
Q3: If I cough occasionally when eating, does that mean I’m still healing?
Yes—it can mean your swallowing is still recovering. But you should mention it to your therapist because it may indicate aspiration risk or need for adjustment in diet or exercises.
Q4: Are there specialised centres for swallowing recovery in Honolulu?
Yes. If you look for “Choke Stroke Treatment Honolulu” or swallowing rehab services tied to stroke recovery, you can find facilities specialising in this area. It’s worth asking for referrals.
Q5: How long should I expect improvement to continue?
Most improvement happens in the first weeks to months (1-4 weeks to 3-6 months). But continued improvement can happen up to 12 months or more with consistent therapy and support.